At Legion Healthcare Partners we specialize in the prior authorization process. We have developed a unique approach to the approval process. This approach will teach your organization how to adequately obtain approvals for your organization.
Assessment
We will start by reviewing your current process and documenting areas that are performing well and areas of improvement. In addition, we will review your claim denials for trends related to prior authorization. By analyzing your current data, we will establish baselines for your insurance submission process and patient service appointments, which ultimately leads to faster care.
Strategy
Rather than taking a submit and see what happens approach our team compares the clinical notes of the patient to the medical policy and benefits in an attempt to demonstrate medical necessity during the initial submission. Our team understands state and federal administrative code and what is expected of the health plan. We use that information to strategize on the best way to get to an approval. In addition, we use highly trained clinical staff, that can articulate the clinical needs of the patient during the appeal process.
Understanding Benefits
We go beyond just understanding a patient’s co-pay balance. We focus on understanding the structure of the health plan, from self-funded to fully funded, where claims and prior authorizations are processed and what information will be needed when and if there is a problem obtaining the authorization.
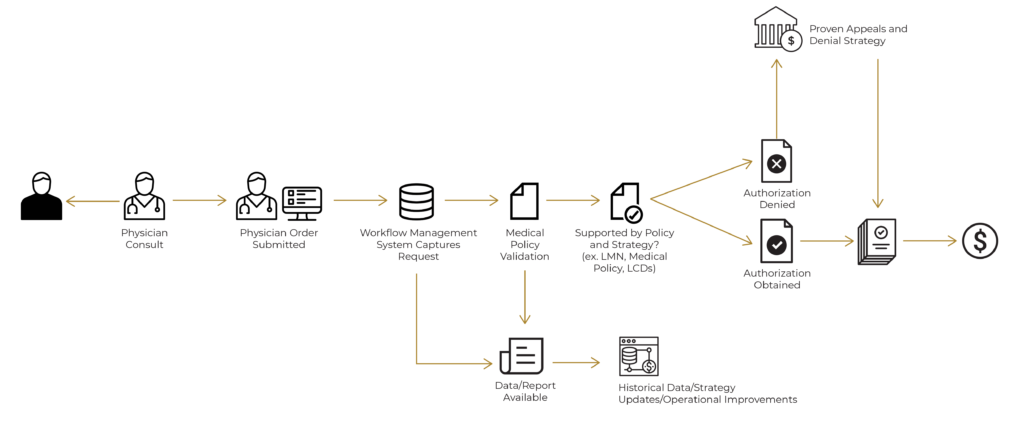
Legion uses a collaborative style that teaches your team how to huddle daily to discuss cases and can implement a workflow management system that can be transparent to your physicians and administrative staff.
Our Strategy
The strategy of Legion Healthcare Partners is to improve your prior authorization operations as quickly as possible and to capture as much additional revenue by improving documentation, prior authorization process, correct coding, ensure proper payment, and help address backend claim denials. We will also ensure that all clinical staff that drop charges are adequately trained and this person will serve as a resource if anybody has any billing and coding questions.
Our services include:
- Intake, Referral Management, and Prior Authorization Assessment and Development Plan
- Prior Authorization Management Services – Daily management of prior authorization activities to include strategy, staffing, operations, appeals/denials
- Prior Authorization Assistance – Assist with staffing shortages, high volume, complex cases or any other scenario
- Providing an Intake and Prior Authorization Workflow Management Suite
At Legion Healthcare Partners, our process stands above competitors in two areas. First, we know the top claim denial reason is “No Prior Authorization Required,” and we understand the deficiencies in obtaining prior authorizations cost organizations hundreds of thousands of dollars every year. We employ tactics that force payors to provide an authorization and/or we provide supporting documentation for the no prior authorization required reason. Second, we don’t just take over your prior authorization process and leave you in the dark. We work with existing team members to train to our standards and can also train incoming staff. We ensure that at the end of a contract, your staff will understand how to properly process an authorization and reduce claim denials.
Our Expertise
- Strategic Operational Redesign for Successfully Navigating Prior Authorization Barriers at a Large Volume Proton Therapy Center (JCOP, 2020)
- Three-Year Results of a Prospective Statewide Insurance Coverage Pilot for Proton Therapy: Stakeholder Collaboration Improves Patient Access to Care (JCOP, 2020)
- Cost-Effectiveness Models of Proton Therapy for Head-and-Neck: Evaluating Quality and Methods to Date (IJPT, 2020)
- The Insurance Approval Process for Proton Therapy: A Significant Barrier to Patient Care (IJROBP, 2017)
- The Proton Insurance Approval Process for Thoracic Patients: Metrics and Access (IJROBP, 2017)
- Insurance Approval for Proton Therapy for Head and Neck Cancer: One Cancer Centers Experience (IJROBP, 2017)
- Variations in Proton Therapy Coverage in the State of Texas: Defining Medical Necessity for a Safe and Effective Treatment (IJPT, 2015)
- How Do We Define the Cost of Advanced Technology in Healthcare: A Pilot Study of Proton and Photon Therapy in Oropharyngeal Cancer Patients. (IJOBP, 2015)
- Improving Patient Access to Proton Therapy with Stakeholder Collaboration: University of Texas MD Anderson Cancer Center Pilot Study (NAPT Webinar, 2020)
- Novel Strategy to Reduce Delays, Denials and Administrative Cost for the Proton Therapy Prior Authorization Process (NAPT Conference, 2019)
- Evidence-Based Access to Proton Therapy Does NOT Result in Overutilization: 3-Year Results of a State-Wide Employer-Based Insurance Coverage PILOT (ASTRO, 2019)
- Better Outcomes with Lower Costs: The High Value of PBT Coverage (NAPT Conference, 2019)
- Reducing Delays, Denials and Administrative Cost to Improve Access to Care in Radiation Oncology: The Value Proposition of an Advanced Practice Dosimetrist (SROA, 2019)
- Proton Therapy Authorization Process: Project Update (NAPT Conference, 2017)
- Variations in Proton Therapy Coverage in The State of Texas: Defining Medical Necessity for a Safe and Effective Treatment (NAPT Conference, 2016)
- Proton Therapy Authorization Process | MD Anderson Experience (NAPT Conference, 2015)
We know it can be difficult to visualize what these changes look like for your organization. That’s why we are offering a free consultation. We can set up a time where we look at a case you are having difficulty with and advise on best practices to help get your case overturned.

ABOUT US
By definition, the word Legion means an immeasurable crowd, vast host, multitude or number of people. Our Legion takes the fight against cancer to heart.
SITEMAP
CONTACT US
2001 Kirby Drive
Suite 1100
Houston, Texasinfo@legionhp.com
650-600-0001
FOLLOW US
Images courtesy of Varian Medical Systems. © 2021 Legion Healthcare Partners.

